Designer & Engineer

A-A G
Create Your First Project
Start adding your projects to your portfolio. Click on "Manage Projects" to get started
Project Title
Project Type
Photography
Date
April 2023
This is where the project description goes. Give an overview or go in depth - what it’s all about, what inspired you, how you created it, or anything else you’d like visitors to know. To add Project descriptions, go to Manage Projects.
Air-Armor Gown
Client
Role
Time
Date
Confidential
Project Lead
10 Weeks
November 2023
The Air Armor hospital gown merges soft robotics, sensor communication, and micro air pumps, aiming to safeguard patients from fall injuries by enabling support during mobility and discreetly adapting when they return to their beds.



Patient falls constitute the most prevalent adverse incidents documented in hospital settings. Annually, there are an estimated 700,000 to 1 million instances of patient falls within U.S. hospitals, leading to approximately 250,000 injuries and up to 11,000 fatalities. Roughly 2% of hospitalized patients experience at least one fall during their stay. The occurrence of inpatient falls imposes substantial physical and economic strains on patients. Despite the implementation of numerous guidelines and protocols by hospitals to mitigate fall-related injuries, situations often necessitate nurses to swiftly intervene to prevent these incidents.
The situation is dire.

In 2022, falls accounted for 42% of all adverse events in hospitals, and has been steadily increasing each year.

In hospital fall injuries annually lead to up to 11,000 deaths and 250,000 injuries.
The solution is nuanced.
The solution cannot be age, gender, or body type restricted. There is a wide range of fall risk patients.
Universal
1
The solution must be able to integrate seamlessly into the hospital’s established gown sanitization processes.
Sanitizable
2
The solution cannot rely fully on the nursing staff. Its purpose is to offer some relief to nurses and stop injury when they cannot physically be there.
Automated
3
The solution must not adversely affect the patient’s physical or mental state. Failure to do so could result in bed sores or sleep trouble.
Comfortable
4
Air-Armor System
An air bladder is integrated into a hospital gown and only inflates when a patient passes the set distance between the sensors in their gown and their bed.
This system is specifically designed to be unintrusive and virtually disappear when the patient is lying in their bed. The Air bladder uses soft robotics to autonomously move into position when inflated and eliminate injuries from occurring in the head and hips.
Sensor-driven soft robotics.

Each diamond hinge vertex creates a fold in the air bladder, manipulating it into position when fully inflated.
The head guard protects against brain trauma on the back and sides of the head.
Inlet for the Air Pump Assembly.

Ribbed slits mold around each patients hip when inflated
Diamond hinge hugs the spine and reduces the amount of air needed for protection.


The Circuit
Triggering Inflation and Vacuum.
Ultrasonic Sonar Sensor
HC SR-04

Triggers inflation or vaccuum by measuring the distance from the bed to the patient, as the patient is getting up.
When the sensor reports the distance is over the 24 inches the air bladder inflates.
Arduino
Uno Rev3

A Single-board microcontroller (SBMCs) used to program hardware using C++ scripts via Arduino IDE.
Radio Frequency Transmitter
433 MHz

By utilizing a sequence in the Arduino IDE script, Radio Frequency Transmitters and recievers can sync ultrasonic sensors data to communicate with other ultrasonic sensors.
Used with multiple sensors giving a better reading on where the patient is in the hospital room.
Two Mini Air Pump
5V-6VDC, 100 KPa 370

Inflates and Deflates the protective air bladder in the gown.
When the ultrasonic sensor reads that the patient is getting up and walking, it will keep the air bladder inflated to prevent injury.
Lithium Ion Battery
7.2V, 1500mAh

A rechargable power source for nurses to easily track and maintain the full operation of the Air-Armor Gown.
Arduino
Single Sensor Sketch
When only using the sewn-in ultrasonic sensor, this script triggers inflation and deflation of the gown's air bladder system.
#define echoPin 7 // Echo Pin
#define trigPin 8 // Trigger Pin
#define rfTxPin 9 // rf Transmit enable
#define inflPin 10 // Inflate Pin
#define vacPin 11 // Vacuum Pin
#define LEDPin 13 // Onboard LED
#define BitPeriod 500 // Bit period for RF sync bits in microseconds
boolean syncSeq[16] = {1, 0, 1, 0, 1, 0, 1, 0, 1, 0, 1, 0, 1, 0, 1, 1} ; // Bit sequence for synchronization
int maximumRange = 30; // Maximum range needed (cm)
int minimumRange = 0; // Minimum range needed
long duration, distance; // Duration used to calculate distance
long timeout = 50000; // Ping duration timeout (uS)
unsigned long previousMillis = 0;
const long inflateTime = 10000;
unsigned long previousvMillis = 0;
const long vacuumTime = 10000;
void setup() {
Serial.begin (9600);
pinMode(trigPin, OUTPUT);
pinMode(echoPin, INPUT);
pinMode(rfTxPin, OUTPUT);
pinMode(inflPin, OUTPUT);
pinMode(vacPin, OUTPUT);
pinMode(LEDPin, OUTPUT); // Use LED indicator (if required)
digitalWrite(trigPin, LOW);
digitalWrite(rfTxPin, LOW);
digitalWrite(inflPin, LOW);
digitalWrite(vacPin, LOW);
}
void loop() {
digitalWrite(inflPin, 0);
digitalWrite(vacPin, 0);
digitalWrite(LEDPin, HIGH);
TxRFSync() ; // Send RF synchronization sequence
digitalWrite(trigPin, HIGH); // Start ping sequence
delayMicroseconds(10);
digitalWrite(trigPin, LOW);
duration = pulseIn(echoPin, HIGH, timeout);
digitalWrite(LEDPin, LOW);
unsigned long currentMillis = millis();
unsigned long currentvMillis = millis();
//Calculate the distance (in cm) based on the speed of sound.
distance = duration / 58.2;
if (distance >= maximumRange || distance <= minimumRange)
{
/* Send a negative number to computer */
Serial.println("-1");
if (currentMillis - previousMillis >= inflateTime)
{
if (inflPin == HIGH)
{
digitalWrite(inflPin, LOW);
}
}
else
{
digitalWrite(inflPin, HIGH);
}
previousvMillis = currentvMillis;
}
else {
/* Send the distance to the computer using Serial protocol. */
Serial.println(distance);
if (currentvMillis - previousvMillis <= vacuumTime)
{
if (vacPin == HIGH)
{
digitalWrite(vacPin, LOW);
}
else
{
digitalWrite(vacPin, HIGH);
}
}
previousMillis = currentMillis;
}
//Delay 100ms before next reading.
delay(100);
}
// Function to write "syncSeq" bit sequence to RF transmit port
void TxRFSync()
{
for (int k = 0; k < sizeof(syncSeq) ; k++)
{
digitalWrite(rfTxPin, syncSeq[k]) ;
delayMicroseconds(BitPeriod) ;
}
digitalWrite(rfTxPin, LOW) ; // Turn off transmit at end of sequence
}



A common place for fall injuries to occur in hospitals is on the way to the bathroom. Patients may misjudge their strength and believe that their state is unaltered from medication or the original injury.
Patient protected going to the bathroom.
Gown is inflated when the sensor detects the patient's back is 24 inches off the bed (sitting up in the bed)
Deflate Zone
Getting to the Final Prototype.
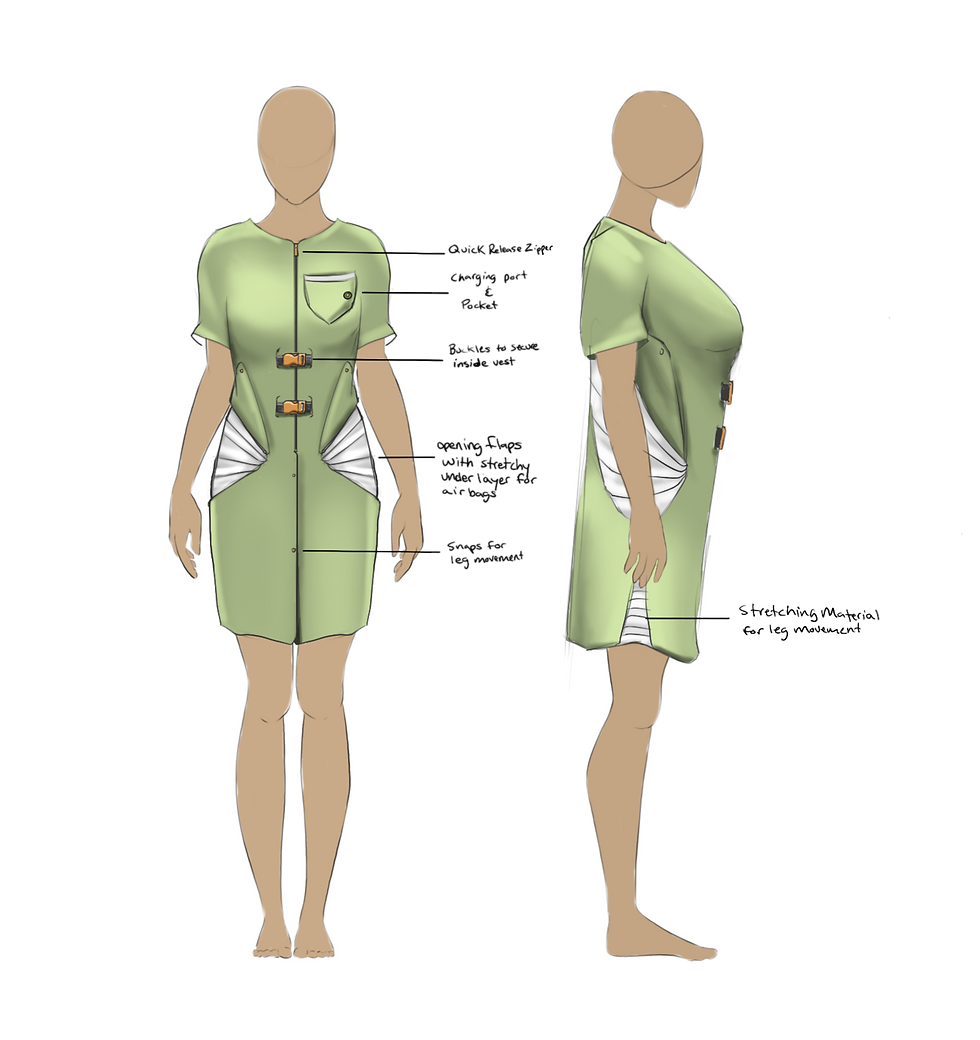
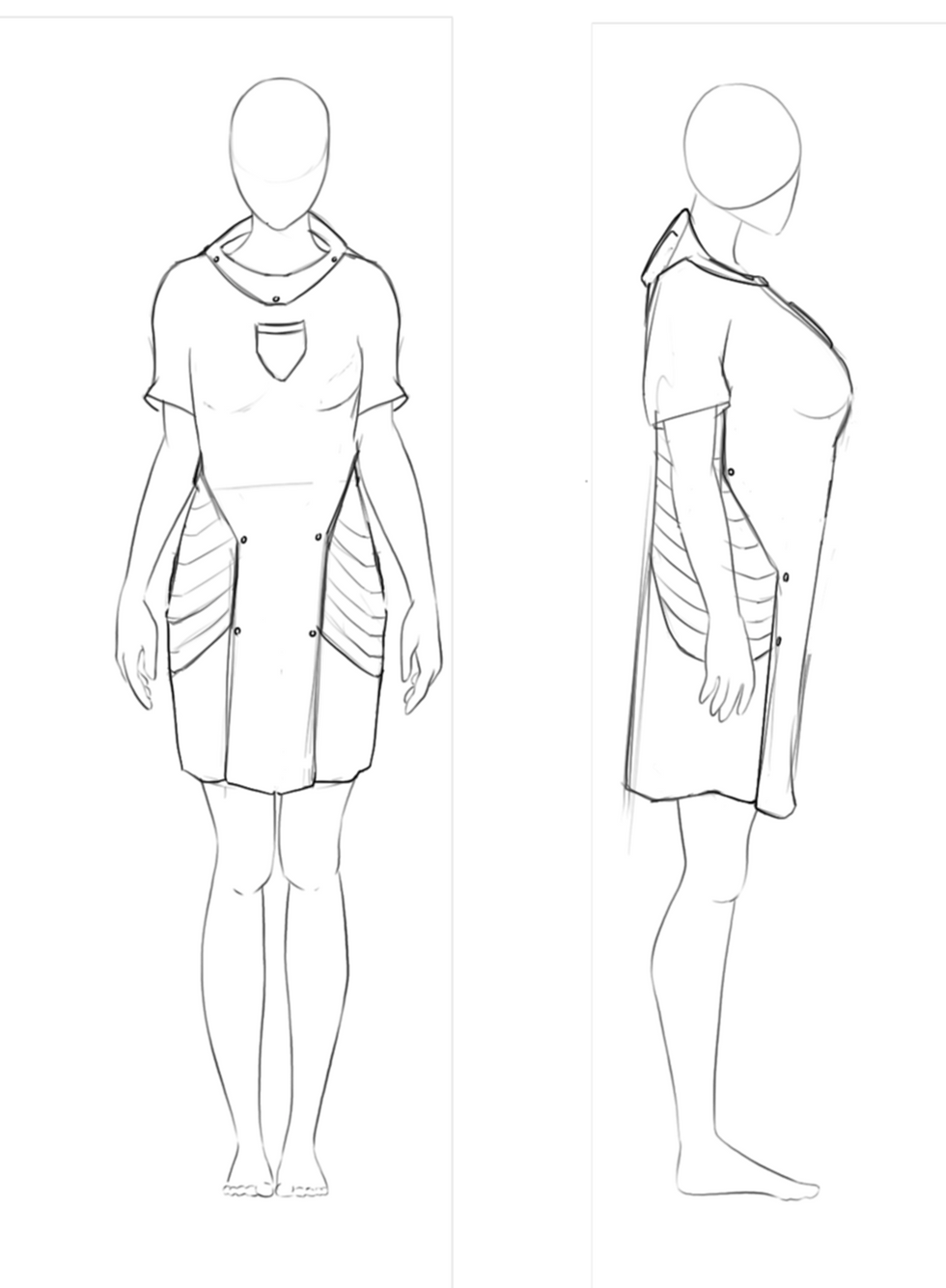
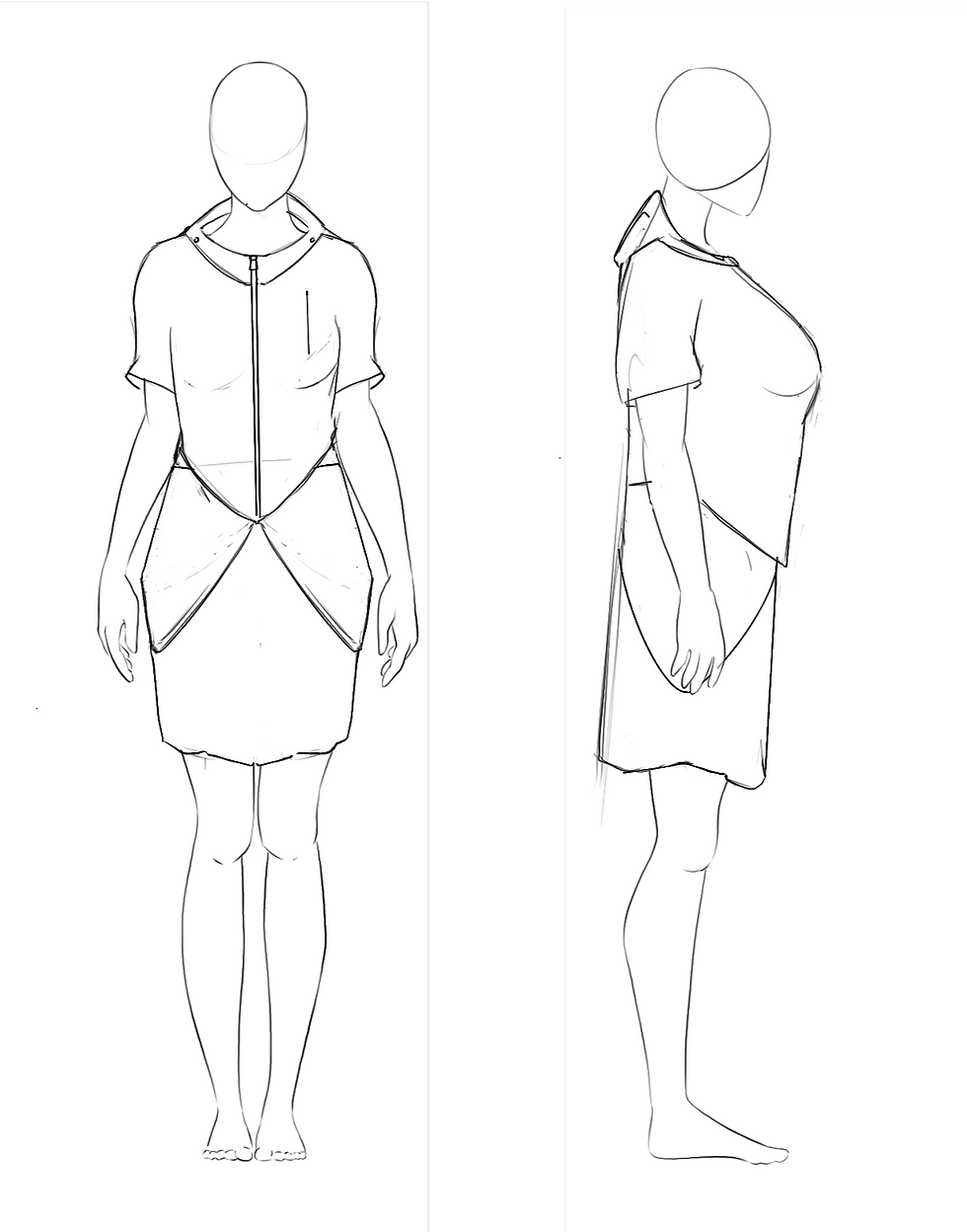
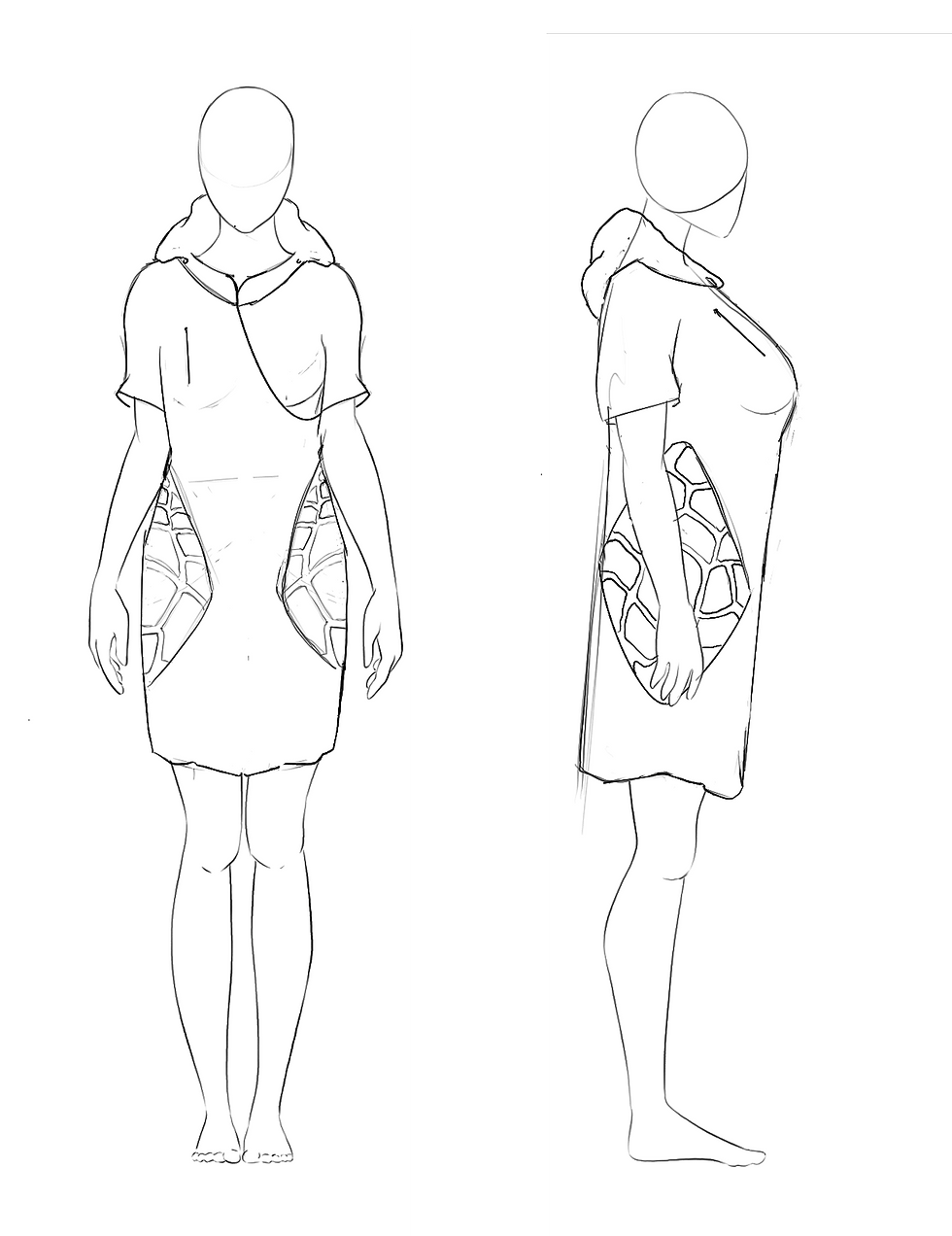
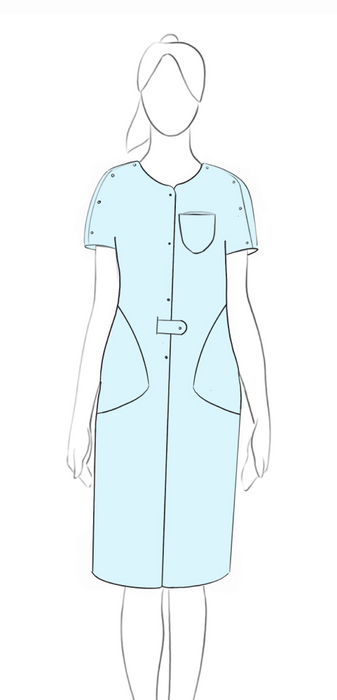
After conducting a thorough investigation of the problem and formulating four main attributes that the solution must achieve, the team proceeded with ideation sketches. Sketching, as a means of brainstorming, aids in materializing abstract ideas and communicating the proposed solutions to the rest of the team.
1. Initial Sketches

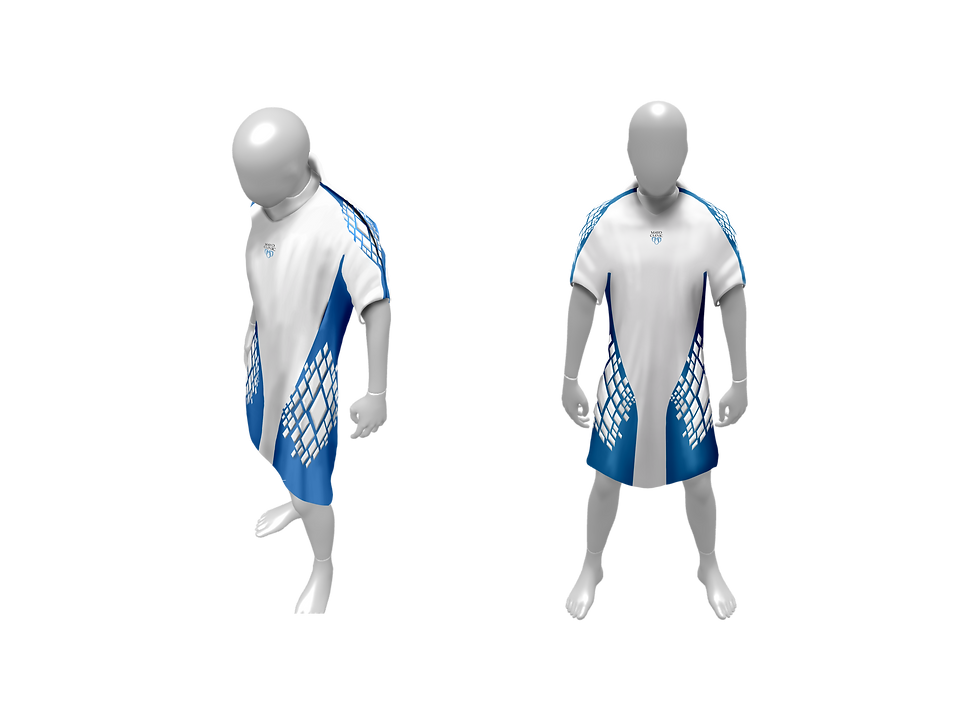
After the team met and discussed our initial sketches, we outlined the emerging ideas, encompassing both minor details and overarching concepts. At this stage of the design process, it's crucial not to dismiss any potential concepts, regardless of their scale. With this compiled list of ideas earmarked for further exploration, I established parameters in an AI diffusion-style model. Utilizing the aforementioned initial sketches as control images, this approach swiftly visualized our ideas, offering insights into their potential applications in prototyping.
2. AI Generative Ideation
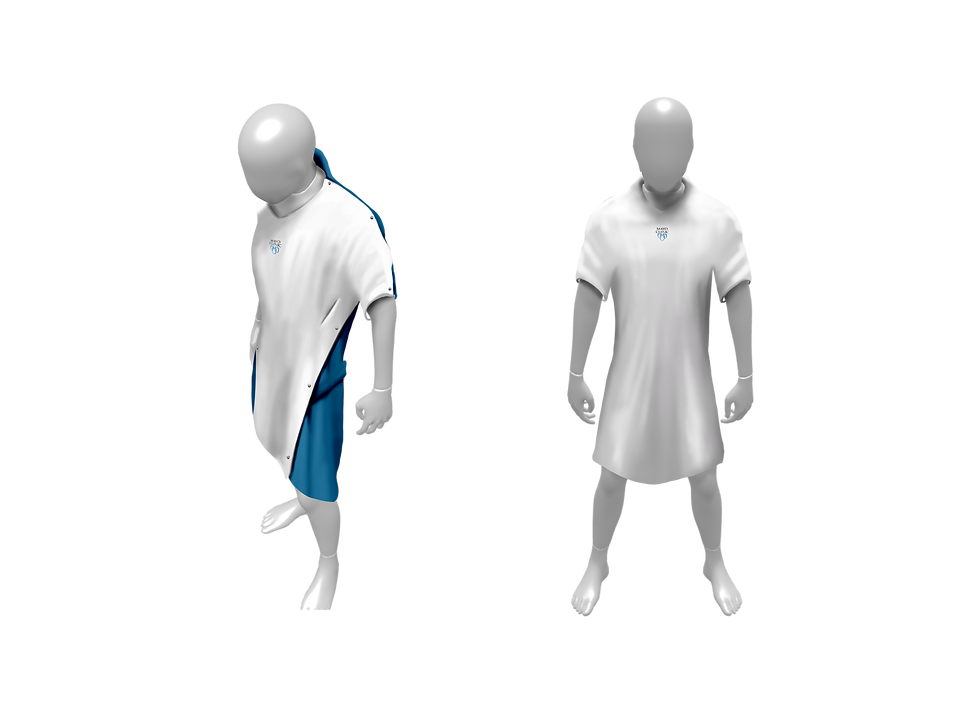
Mayo Clinic initially tasked us with designing a gown to accommodate existing products, aiming to accelerate the timeline and swiftly implement a functional solution to prevent further injuries.
After primarily testing the S Airbag Vest, we discovered its unsuitability for hospital use due to several reasons: it relied on two proprietary helium canisters for each deployment, produced excessive noise, exhibited inconsistent deployment, and required complete disassembly for sanitation. Additionally, relying on a sensor to detect patient falls proved inconsistent, prompting us to pursue a continuous protection solution for at-risk patients.
What was learned.
Experimenting with various materials, we explored 3D printing gyroid structures from TPU and created molds for silicone and flexible polyurethane. These were strategically oriented on optimized impact area maps to reduce the required padding.
Developing static solutions with optimized padding aimed to eliminate reliance on electricity, easing the burden of gown charging and removing hardware malfunctions. However, while potentially applicable to less at-risk patients, this approach proved uncomfortable due to substantial padding requirements, particularly for patients lying in bed. It was obtrusive and necessitated additional headgear for effective head protection.
What was learned.
Experimenting with the air bladder system was an iterative process. For rapid prototyping, we utilized a flat iron, parchment paper, and heat transfer vinyl, facilitating the testing of various hinge and shape designs tailored to different parts of the patient’s body.
The use of air bladder hinges allowed the protection system to adapt to the correct shape upon inflation and return to its original form when deflated. This functionality ensured adequate protection when necessary while causing minimal disruption when not in use. This approach aimed to provide a comfortable experience for patients lying in bed, preventing additional injuries such as bed sores and offering the sensation of wearing a normal gown.
What was learned.
Overview.
Unintrusive, Hands Free Protection
The Air Bladder is sewn into the gown and can withstand sanitization processes
Air Bladder

Hugs when inflated to insure proper coverage of each patients hip.
Hip Padding
Easily Removable and Faces backward to get the best reading when the patient is getting up.
Ultrasonic Sensor
The Circuit is tucked up in the inner arm to minimize discomfort while lying down.
Circuit Pouch
The whole gown can be split in half by pulling on the collar.
Shoulder line Snaps

The head guard protects against brain trauma on the back and sides of the head
Head Cover
Ribbed slits mold around each patient's hip when infalted
Hip Padding
Hinge vertex creates folds in the air bladder, manipulating it into position when inflated
Main Hinges
Air pump inlet is located in the ideal location for patient comfort.
Air Inlet
Diamond hinge hugs the spine and reduces the amount of air needed for protection.
Spine Channel

Head Cover and Main Hinges

Spine Channel and Hip Protection